As I reevaluate my theory, I have come full circle in my research and came across the research paper entitled:
The Role of Regulatory T Cells in Cancer
Tai-You Ha*
Department of Immunology, Chonbuk National University Medical School, Chonju, Chonbuk, Korea
The Role of Regulatory T Cells in Cancer

I postulate that the T regulatory cells may be the major stumbling block in the whole immunotherapy.
Recent studies have shown that CD4+CD25high FoxP3+ Treg cells are overrepresented in human metastatic lymph nodes with a 2-fold increased frequency
compared with both tumor-free lymph nodes and that advanced melanoma is associated with increased numbers of circulating Treg cells and Dendritic Cells (DCs) and suggested that melanoma induces immunosuppressive DCs and Treg cells in the systemic circulation of the patients . Vence et al also showed the presence of tumor antigen-specific CD4+ Treg cells in the blood of patients with metastatic melanoma.
This means the host (you) may already have the correct antigen, but the tumor and microenvironment may be suppressing the immune response by secreting suppressive cytokines like TGF- beta , IL-10, and IL -6 and or proliferating the suppressive Tregs.
Nicholaou et al most recently showed in patients with melanoma that although strong antibody responses were mounted, the generation of delayed-type hypersensitivity response was significantly impaired and patients with advanced melanoma had a significantly higher proportion of circulating CD4+ CD25+FoxP3+ Treg cells compared with those with minimal residual disease. So we now can blame the tolerance of our immune system to cancer on the T Regulatory Cells (Tregs).
It has been reported that the large number of different cell types that are claiming to be directly targeted by FoxP3+ Treg cells are CD4+, CD8+ T cell, dendritic cells, B cells, marophages, osteoblasts, mast cells, NK cells, and NKT cells.

No wonder our immune system can’t raise an attack on the Melanoma. The tumor is like a castle in the middle ages. The castle (tumor) is surrounded by a moat the (suppressive cytokines) and the walls and towers are the Tregs. If you take out walls and tower, the castle becomes vulnerable.
These Tregs when activated, upregulate the CTLA-4, CD25 (IL-2), and other receptors. So if you control the function of the Tregs, you may be able to break the tolerance of the immune system. This can be done by blocking receptors on the Treg cells

It was also noted as the tumor burden increased, so did the Tregs in the peripheral which makes it harder to eradicate tumors in the advanced stage of Melanoma.

Wieczorek et al found that Treg cell numbers are significantly increased in the peripheral blood of patients with IL-2-treated melanoma. IL-2 stimulates CXCR4 expressed on the Tregs enables the Tregs to migrate CxCL12 in the tumor microenvironment increasing the Treg accumulation.
So we need to deplete, block and limit the expansion of the Tregs. We also want to limit the concentration of Interluekin-2 at the early stage of the CD4+ T-cell expansion. This can be done in a number of ways, but why not use an antibodies that can indirectly accomplish both tasks at once. By using anti-CTLA-4 blockage we keep the activation going, causing a free for all for the cytokine IL-2 that is secreted.
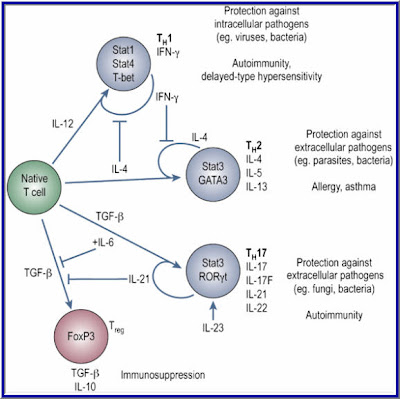
CD4+ T cells regulate immune responses by producing various cytokines upon antigen stimulation. Naive CD4+ T cells have limited cytokine responses and secrete only IL-2 before they differentiate into various effector cell types CD4+ T cells regulate immune responses by producing various cytokines upon antigen stimulation. Each cell type is competing for a limited amount of IL-2 secreted by a small subset of the T helper cells. Naive T cells stimulated with antigen in the presence of IL-4 differentiate into Th2 cells secreting IL-4, IL-5, IL-10, and IL-13, whereas IL-12 induces the differentiation of naive cells into Th1 cells secreting IL-2, IFN-γ, and lymphotoxin.
FROM:
Autoimmunity: IL-21: a new player in Th17-cell differentiation
Elissa K Deenick and Stuart G Tangye
WWW.Nature.com
Ribas and Restifo et al found that if you use Anti-CTLA-4 blockade the native T-cell is pushed towards the Th17 differentiation. This causes less interleukin-2 to be produced by the CD4+ T-cells causing a shortage of IL-2 in the microenvironment for the expanding T-cells thus limiting the differentiation to Tregs. It is well known that in the presence of TGF-beta and IL-2, the Native T-cell differentiates into T Regulatory Cells.
Also the activation and differentiation of Naïve CD8+ T cells require IL-2 provided by activated CD4+ T cells at the initial priming stage within 0–2.5 hours after stimulation. Thers is
critical IL-2 signal from CD4+ cells is mediated through the IL-2R (receptor) of Naïve CD8+ cells. This activation of IL-2 signaling advances the restriction point of the cell cycle, and thereby expedites the entry of antigen-stimulated Naïve CD8+ T-cell into the S phase of the cell cycle.
The cell cycle has four stages:
1. G1 phase when the cell increases in size and gets ready to replicate its DNA.
2. S phase when the cell synthesizes or copies its chromosomes
3. G2 phase in which the cell prepares to divide
4. M phase when mitosis occurs.
If no IL-2 is available to Naïve CD8+ T-cells, they never get a chance to expand and differentiate into Cytotoxic T Lymphocytes (CTLs) Killer T-cells.
Besides promoting cell proliferation, IL-2 stimulation increases the amount of IFNγ and granzyme B produced by CD8+ T cells.
Activation and Differentiation of (CTLs) Cytotoxic T Lymphocytes
Naïve CD8+ T-cells are referred to as CTL-precursors (CTL-Ps), which are incapable of performing any function other then recognizing the class I MHC-antigen complex on the Tumor cells through the (TCR) T Cell Receptor.
For activation, the CTL-P needs at least three signals:
1. Antigen specific signal transmitted by the MHC I peptide/TCR complex for the recognition of the Antigen
2. The Costimulatory signals transmitted by the CD28 receptor and the B7 molecule of the Antigen Presenting Cells (APCs)
3. Cytokine induced signal, IL-2 interaction with the IL-2r (receptor) on the CTL-P leading to activation and differentiation of the CTL-P into effector CTL
The Cytokine IL-2 came from the(CD4+) TH1 cells which means the CTL-P is IL-2 limited and can only be activated by the secreted IL-2 if there is any to be had or by introducing IL-2 through IL-2 therapy. Now you know the reasoning behind using the IL-2 therapy as the second part of the combinatorial Therapy. If there is not enough IL-2 in the host environment, you will only get partial expansion of the CTLs. It may not be enough to eradicate large bulky tumors.
The Interluekin-2 plays another role in this Melanoma Maze. In a study by Janas et al, Il-2 increases the expressions of the perforin and granzyme A, B and C genes in the CD8+ T-cells. This increase expression causes the CD8+ T-cells to mature into Cytoxic T Lymphocytes (CTLs). The exogenous IL-2 is required for the granzyme proteins. CTLs have cytoplasmic granules that contain the proteins perforin and granzymes. A dozen or more perforin molecules insert themselves into the plasma membrane of target cells forming a pore that enables granzymes to enter the cell. Once in the tumor cell, these enzymes are able to breakup (lyse) the cell and destroy it. This is the beginning of the end for the cancer cells. The tumors begin to shrink and the rest is history.
Research suggests that the primary mode of the destruction of the tumors by CTL is by initiating death through the Fas-FasL pathway. Studies have shown that CTLs store Cytotoxic proteins in the form of granules in their cytoplasm.
These proteins belong to two categories:
1. Perforins: involved in pore formation
2. Granzymes: responsible for hydrolysis of the cellular products.
Granzymes breaks down the tumors cells just like your detergent enzymes in your laundry detergent.
Immediately following a CTL contact with the tumor cell, the Golgi sacks load with granules and granzymes which create pores to allow the granzymes to enter and destroy the tumors cells.
So now you know why Anti-CTLA-4 blockage and HD Interluekin-2 go hand and hand. Timing of the addition of IL-2 can make or break the immune response. And without suppressing the Tregs, your chances to mount an immune response may be slim at best. Your Immune System is a well Orchestrated system of events; we just need the Knowledge on how to harvest its potential on eradicating cancer.

The beginning of knowledge is the discovery of something we do not understand.
~Frank Hebert~
A critically acclaimed and commercially successful American science fiction author
Take Care,
Jimmy B






I will be very appreciate for you article. According to the biological significance of lymphocyte recirculation, why is T cells recycle faster than that B cells?
ReplyDeletecdna