Bristol-Myer Squibb Pharmaceutical Research Institute
Attention: Elliott Sigal
Route 206, Provinceline Road
P.O. Box 4000
Princeton, New Jersey 08543 U.S.A...
Date: 3-10-2010
Attention: Elliott Sigal
Route 206, Provinceline Road
P.O. Box 4000
Princeton, New Jersey 08543 U.S.A...
Date: 3-10-2010
Dear Dr. Sigal:
I want to thank you for responding to my emails over the last few months. I know I can be candid and straight to the point sometimes. By reopening the compassionate Drug Use (ipilimumab) you and your company gave the Melanoma Patients “The Last Chance of HOPE”. You don’t know how much this means to us. If we haven’t passed the “Lethal Tumor Burden” we still have a chance of survival. I believe you have done your company justice and showed your compassion. My faith in the Company’s Ethics has been restored.
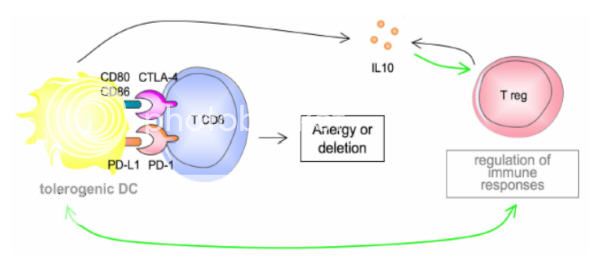
Now we need to prove to the world that this drug may be one of the most important discoveries in the last twenty years of Cancer. By taking the “Brakes off the Immune System” we can harness our own immune system to battle cancer. Granted we may have to use the drug in combinatorial therapy to rid the host of the cancer once and for all. I hope you and your company can collaborate together with all the major players in this exciting field of Oncology. See it took millions of years for our immune system to evolve, so why do we think that one drug can do it all. We need to approach the Beast arm to arm, to block all the pathways so it can’t escape. This can only be done by using one’s own immune system.
Can you imagine working out a protocol that will vaccinate the patient with the patients own tumor–specific antigen? And Ipilimumab (Anti-CTLA-4 Blockade) is at the center of this revolutionary therapy/protocol. Please if you get a chance, listen to some of the lectures and symposiums from the like of Dr. James Allison, Dr. Jedd Wolchok, Dr. Antonio Ribas, Dr. Jeffery Weber, Dr Keith Flaherty and others. You will be amazed at their accomplishments in the clinical setting. But they need more. They need access to the entire drug arsenal that is available across companies. We now know that timing and dose concentration plays a major roll in setting up an immune response. There are feedback loops. It is like dominos. You have this elaborate step-up. It may take weeks to build. Once you set it in motion, the chips begin to fall. There are different pathways, cytokines, T-cells, receptors, etc that need to be taken into account get the right immune response. This immune response can only be generated if you have all the keys to unlock the response. We need yours and other Pharmaceuticals to work together for the good of the cancer patients. We need to take down all the red tape which also includes the FDA.
“Our Life depends on it.”
Thanks again.
Sincerely,
Jim Breitfeller
I want to thank you for responding to my emails over the last few months. I know I can be candid and straight to the point sometimes. By reopening the compassionate Drug Use (ipilimumab) you and your company gave the Melanoma Patients “The Last Chance of HOPE”. You don’t know how much this means to us. If we haven’t passed the “Lethal Tumor Burden” we still have a chance of survival. I believe you have done your company justice and showed your compassion. My faith in the Company’s Ethics has been restored.
Now we need to prove to the world that this drug may be one of the most important discoveries in the last twenty years of Cancer. By taking the “Brakes off the Immune System” we can harness our own immune system to battle cancer. Granted we may have to use the drug in combinatorial therapy to rid the host of the cancer once and for all. I hope you and your company can collaborate together with all the major players in this exciting field of Oncology. See it took millions of years for our immune system to evolve, so why do we think that one drug can do it all. We need to approach the Beast arm to arm, to block all the pathways so it can’t escape. This can only be done by using one’s own immune system.
Can you imagine working out a protocol that will vaccinate the patient with the patients own tumor–specific antigen? And Ipilimumab (Anti-CTLA-4 Blockade) is at the center of this revolutionary therapy/protocol. Please if you get a chance, listen to some of the lectures and symposiums from the like of Dr. James Allison, Dr. Jedd Wolchok, Dr. Antonio Ribas, Dr. Jeffery Weber, Dr Keith Flaherty and others. You will be amazed at their accomplishments in the clinical setting. But they need more. They need access to the entire drug arsenal that is available across companies. We now know that timing and dose concentration plays a major roll in setting up an immune response. There are feedback loops. It is like dominos. You have this elaborate step-up. It may take weeks to build. Once you set it in motion, the chips begin to fall. There are different pathways, cytokines, T-cells, receptors, etc that need to be taken into account get the right immune response. This immune response can only be generated if you have all the keys to unlock the response. We need yours and other Pharmaceuticals to work together for the good of the cancer patients. We need to take down all the red tape which also includes the FDA.
“Our Life depends on it.”
Thanks again.
Sincerely,
Jim Breitfeller
responsive to change.”
~Charles Darwin~
Take Care,
Jimmy B